73 year old male with Hyponatremia
THIS IS AN ONLINE E LOG BOOK TO DISCUSS OUR PATIENT'S DE - IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS / HER /GUARDIAN'S SIGNED INFORMED CONSENT .HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH SERIES OF INPUTS FROM AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS WITH AN AIM TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE BASED INPUT
CHEIF COMPLAINTS:
A 73-year-old patient came to the opd with chief complaints of
dizziness and weakness
HISTORY OF PRESENTING ILLNESS:
the patient was apparently asymptomatic 4 to 5 years back then
he went to a local hospital with weakness and was diagnosed with hypertension and
started using MET XL25 tablet under regular medication.
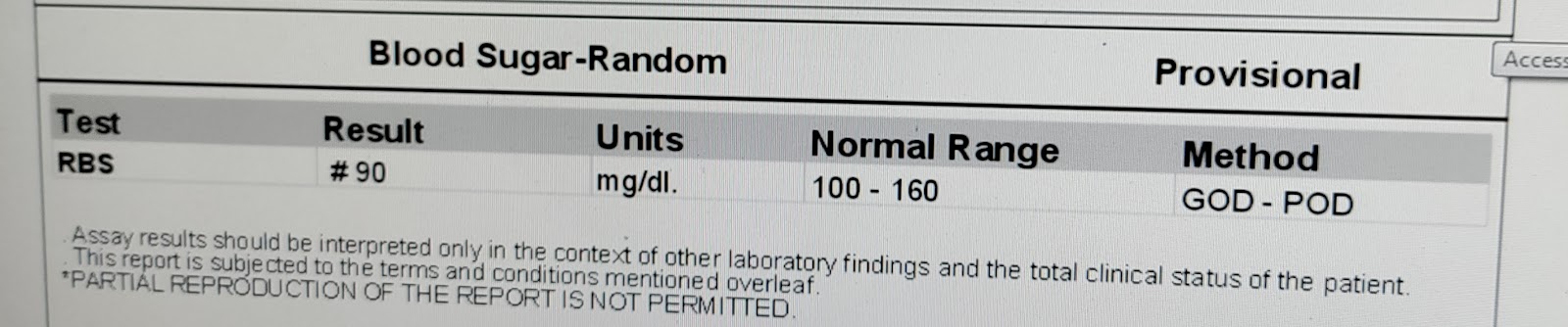
2 to 3 years back patient developed polyuria and went to a local hospital and was diagnosed with type 2 Diabetes mellitus and started Oral hypoglycemic agents.
2 years back he had complained of pain abdomen and was diagnosed with Gall stones then he started using medication and the pain subsided.
1week ago patient developed fever and weakness and skipped lunch and dinner then on next day at around 5am in the morning patient went for urination outside and had a history of fall(slipped). He did not have post-fall loss of consciousness, seizures, and vomiting. Then he walked and slept.
At around 8 am patient could not walk and was taken to a pvt hospital.
At Pvt hospital Investigations were done showing- Hyponatremia and low serum osmolality. 2D echo-with in normal limits
DAILY ROUTINE:
The patient used to be a farmer but stopped working 15 years back due to joint pains and weakness and was mostly confined to his home and surroundings. He wakes up at 5 AM and freshens up.He has breakfast at around 9 am and then rests for some time. He has lunch at 1 pm and rests for an hour. In the evenings he spends time with his family or by himself or chats with the neighbors. He takes dinner at 8 pm and goes to bed.
PAST HISTORY:
No history of TB,CAD,Asthma and thyroid abnormalities
PERSONAL HISTORY:
Diet: mixed
Appetite: normal
Sleep: adequate
Bowel and bladder: Irregular- hard stools once in 3 days and decreased micturition
Habits: none
FAMILY HISTORY:
Not significant.
GENERAL EXAMINATION:
The pt is drowsy on examination
Well oriented to time, place and person
Moderately built and moderately nourished
Pallor – absent
Icterus - absent
Cyanosis - absent
Clubbing – absent
Lymphadenopathy - absent
VITALS:
Temperature – 98.6F
BP - 110/70
HR – 82bpm
RR – 18 cpm
SpO2 – 97%
GRBS -- 105 mg/dl
SYSTEMIC EXAMINATION:
CNS: Patient is conscious
Speech normal
No signs of meningeal irritating
Motor and sensory system- Normal
Reflexes - present
Cranial nerves - intact
CVS: S1 and S2 sounds heard
RS: NVBS +, trachea : Central
ABDOMEN:
INSPECTION
Shape - Scaphoid, with no distention.
Umbilicus - Inverted
Equal symmetrical movements in all the quadrants with respiration.
No visible pulsation, peristalsis, dilated veins and localized swellings
PALPATION
No hepatomegaly
No splenomegaly
ASCULTATION
Bowel sounds present.
INVESTIGATIONS:
PROVISIONAL DIAGNOSIS:
Hyponatremia under evaluation
TREATMENT:







Comments
Post a Comment