I have been given this case to solve in an attempt to understand the topic of "Patient Clinical Data Analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and diagnosis with a treatment plan.
This is an online E log book to discuss our patient’s de-identified health data shared after taking his guardian’s signed informed consent.
A 75 year old male, farmer by occupation and a resident of Miryalaguda presented with chief complaint of lower backache, increased urine output and yellow coloured urine.
HOPI- The patient was apparently asymptomatic 5 years back then he had joint pains of both the knees and low back ache with difficulty in walking for 3 to 4 months with right knee joint swelling. Right knee joint was aspirated.
6 days back he had Pain in lower back which is shooting type continuous and radiating to lower limbs(Pain was severe that he couldn't sit, so they went to a local hospital and got treated).
Pain was followed by fever which is Intermittent, and temperature increased at night and fever subsides by morning. Fever relieved on medication (Dolo).
There is also increased frequency of micturition around 15times in a day(18 times in one night), yellow coloured urine.
No H/o Nausea, vomiting, diarrhoea, headache, dizziness.
Past History - k/c/o DM and HTN since 5 years. Not a known case of TB, Asthma, Epilesy.
Personal History-
Diet- Mixed
Appetite - Normal
Sleep- adequate
Bowel- Normal
Bladder- Increased frequency of Micturition.
Addictions - Smoker at 20 years of age
Smoked for 1 year(1 pack per day) and then he discontinued.
Family History - No significant family history
On Examination -
Patient is conscious, coherent, cooperative.
No pallor , Icterus,clubbing, cyanosis , koilonychia, generalised lymphadenopathy.
No b/l pedal oedema
Oedema of left upper limb- present
VITALS
Temp- Afebrile
Bp-120/70 mm hg
Pulse- 80bpm
RR-16cpm
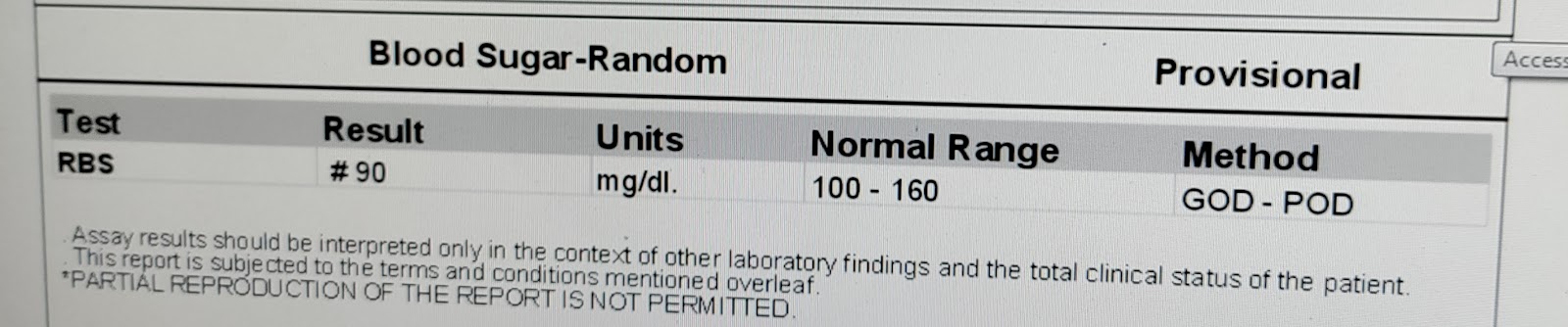
RBS- 121 mg/dl
JVP- raised column of 7cm
Systemic Examination -
Cvs-S1 S2 +
RS- Shape of the chest- Barrel shaped
AP - 85 cms
Transverse - 30 cms
P/A - soft and non tender
CNS-
No meningial signs
GCS:-
Pupils:-
Plantars:- Plantar extensora
Power - Rt Lt
Upper limb- 4/5 4/5
Lower limb- 4/5 4/5
Tone-
Upper limb-. N. N
Lower limb-. N. N
Reflexes:-. Rt. Lt
Biceps. 2+ 2+
Triceps. 2+ 2+
Wrist. 2+ 2+
Knee. 2+ 2+
Ankle. 2+ 2+
Clinical Images
investigations
USG
X-RAY
Provisional Diagnosis -
Spondyloarthropathy
CKD secondary to DM
Diabetes
Hypertension















Comments
Post a Comment