65 year old male with shortness of breath
ROUTINE:
The patient used to be a farmer but stopped working 6 years back due to weakness and was mostly confined to his home and surroundings and sits ideally.
PAST HISTORY:
History of TB 25 years back
Known case of SOB since 2 years
No history of HTN, DM, CAD, Asthma and thyroid abnormalities,epilepsy
PERSONAL HISTORY:
Diet: mixed
Appetite: decreased
Sleep: inadequate due to SOB
Bowel : irregular
Bladder:burning micturition present
Addictions-used to drink alcohol and toddy occasionally -stopped 20 years back
No history of smoking
FAMILY HISTORY:
Not significant.
GENERAL EXAMINATION:
Patient was conscious, cooperative,well oriented to time,place , person. Moderately built and moderately nourished
pallor was present
no cyanosis
no icterus
no clubbing
no generalised lymphadenopathy
no pedal edema
VITALS::
TEMP AFEBRILE
BP 110/70 mmhg
Pulse Rate 78 bpm rhythm(regular)character(normal )
Respiratory Rate :21CPM Abdomino thoracic type
Spo2- ?
SYSTEMIC EXAMINATION:
Abdomen: Soft and non tender. Bowel sounds heard . Skin over abdomen smooth
Shape - scaphoid
Tenderness - no
Free fluid - no
Liver - not palpable
Spleen- not palpable
Cardiovascular system:
INSPECTION:-
Chest appears normal in shape
Apex beat is not visible
PALPITATION:
Apex Beat - diffuse No palpable murmurs (thrills)
ASCULTATION:-
S 1; S 2 heard
Central nervous system: No focal neurological deficits.
Respiratory system:
INSPECTION:
Shape of Chest - normal
Trachea position central
Movements of the chest: Respiratory rate:- 21cpm Type- abdomino thoracic type no accessory muscles involved.
PALPITATION:
No local rise in Temperature and tenderness
Expansion of the chest- equal in all planes
PERCUSSION:
Resonant all over the chest except infraxillary area left side
AUSCULTATION:
Normal breath sounds were heard in all areas except the left infra axillary where there are decreased breath sounds.
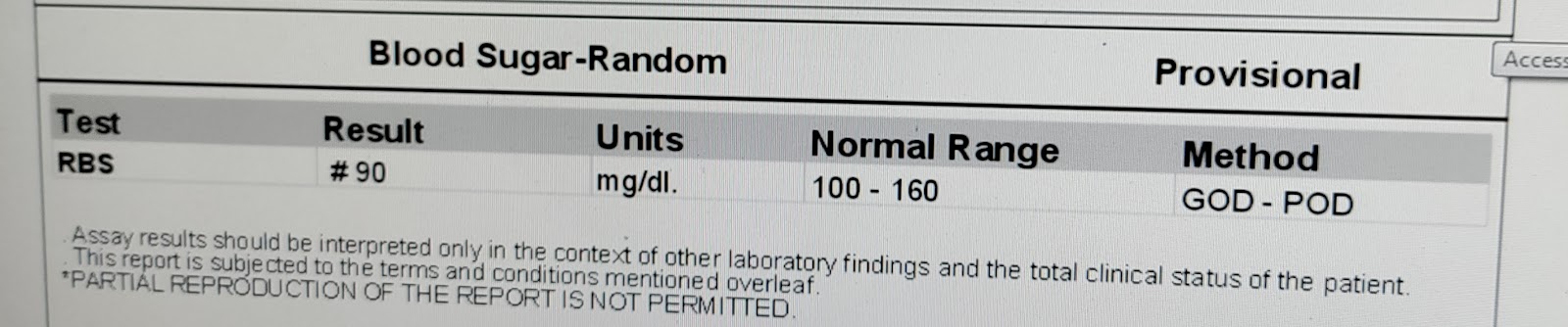
INVESTIGATIONS:
29/11/22
30/11/22
01/12/22
PROVISIONAL DIAGNOSIS:
Pain in the abdomen under evaluation
Heart failure?? with reduced ejection fraction (52%)w
With Anemia under evaluation with Chronic kidney disease
with a history of Pulmonary TB- 20 years back
TREATMENT:
Head end deviation up to 30 degree
supplementation if spo2<90%
MONITOR 4- hrly
NEB - SALBUTAMOL 4 hrly
FEVER CHART 4 th hrly
InJ LASIX 4O mg



























Comments
Post a Comment