27 YR OLD MALE PRESENTED WITH UPPER ABDOMINAL PAIN
THIS IS AN ONLINE E LOG BOOK TO DISCUSS OUR PATIENT'S DE - IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS / HER /GUARDIAN'S SIGNED INFORMED CONSENT .HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH SERIES OF INPUTS FROM AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS WITH AN AIM TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE BASED INPUT
CHIEF COMPLAINTS:
27yr old male ,Mason by occupation resident of vellanki came with chief complaints of upper abdomen pain.
HISTORY OF PRESENTING ILLNESS :
Patient was apparently asymptomatic 3 days ago then he developed stomach pain in epigastric region which is insidious in onset pricking type of pain radiating to back,gradually progressive in nature
It aggrevated on not having food didn't relieve even on taking medication.
He had 1 episode of vomiting on 30/12/22 which is non projectile and non bilious ,with food contents in it.
He had 5-6 episodes of vomiting on 31/12/22.
History of fever 10 days ago.
History of weight loss, loss of appetite, insomnia, fatigue.
No complaints of chest pain, palpitations, SOB, headache, burning micturition,loose stools, giddiness
PAST HISTORY :
He is known alcoholic since 5 years with a daily intake of 180ml.
No history of Diabetes Mellitus, Tuberculosis, Asthma, Hypertension, Epilepsy, Thyroid Disorders.
FAMILY HISTORY :
No significant family history
PERSONAL HISTORY :
Mixed diet
Reduced Appetite
Regular Bowel and Bladder movements
Sleep: inadequate
Alcohol intake regularly around 180 ml daily
Used to smoke but stopped smoking 3years back.
TREATMENT HISTORY:
Tab.Sompraz 40mg
Mucaine gel
Normodorm 25 mg
GENERAL PHYSICAL EXAMINATION :
On examination, patient is conscious, coherent, cooperative
patient is moderately built and moderately nourished
No signs of pallor,icterus, cyanosis, clubbing, lymphadenopathy, generalised edema.
Vitals:
Temperature- afebrile
Pulse rate -68 beats/min
Respiration rate-21cycles/min
BP-130/100mmHg.
SYSTEMIC EXAMINATION:
Abdominal Examination:
INSPECTION:
Umbilicus inverted
No abdominal distention
no visible scars and swelling.
Palpation:
No local rise of temperature
Soft, tenderness present in the epigastric region.
PERCUSSION:
Dullness is present.
Auscultation:
Bowel sounds Heard
Cardio vascular examination:
Apex beat is felt at 5 Intercoastal space medial to mid clavicular line.
S1 S2 heard.
No murmurs.
Respiratory system :
Shape of chest is elliptical, b/l symmetrical.
Trachea is central. Expansion of chest is symmetrical
Bilateral Airway Entry - positive
Normal vesicular breath sounds
CNS examination:
No neurological deficit found.
Gait: normal.
PROVISIONAL DIAGNOSIS:
Alcoholic hepatitis.
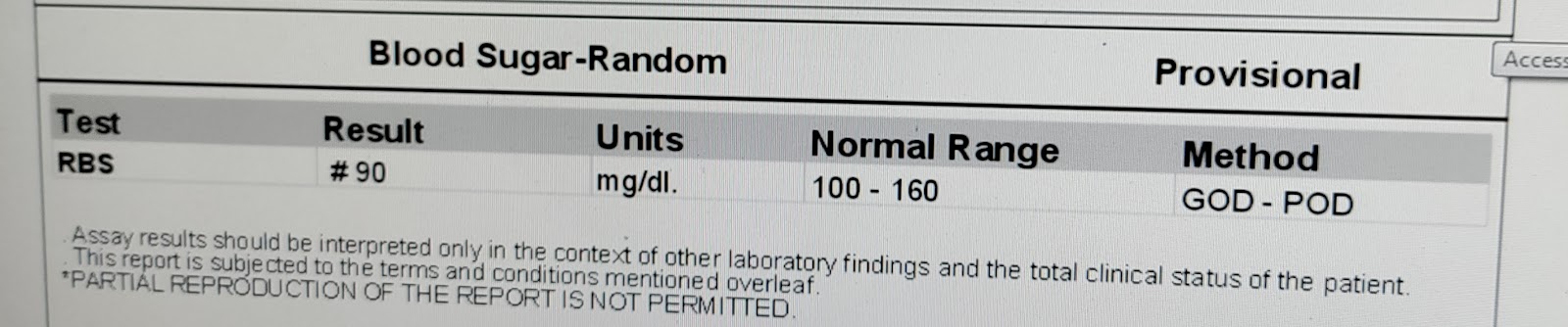
INVESTIGATIONS:
USG:
ECG:

















Comments
Post a Comment