long case 1801006051
THIS IS AN ONLINE E LOG BOOK TO DISCUSS OUR PATIENT'S DE - IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS / HER /GUARDIAN'S SIGNED INFORMED CONSENT .HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH SERIES OF INPUTS FROM AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS WITH AN AIM TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE BASED INPUT
CHIEF COMPLAINTS:
27 year old male patient presented with history of electric shock
HISTORY OF PRESENTING ILLNESS:
The patient was alright 9 months ago.
On July 10th the patient got drunk with friends and was dropped off by his friends nearby his house late at night around 10 p.m.
After some time, his friend passing the road saw him stuck and hugging the pole.
He wasn't responding when called, so his friend tried to pull him away from the pole.
when he tried to touch the pt, he felt an electric shock.
Then he was rushed to a nearby hospital where it was found that he was in cardiac arrest, following which a successful CPR was done, and he was put on a ventilator for around a day.
The Dr noticed that he was in a Vegetative state and referred him to another hospital
At the other hospital, a tracheostomy was done, and he stayed there for 45 days. He contracted an infection with pseudomonas and S. pneumonia and was treated accordingly
All feeding was done through the Ryles Tube.
He was then admitted into another hospital where his condition slightly improved ( able to blink eyes , make eye contact, open mouth) but he was still fed by Ryles tube
He was discahrged and 3 months after the incident he had seizure episodes
No of episodes :- around 10 times
Duration:- 3 to 5 minutes
Treatment given :- Levitarecitam
Patient with his family approached to our hospital to take advice on removal of his tracheostomy tube
PAST HISTORY:
He had several episodes of seizures 3 months after the electric shock.
No history of Diabetes, hypertension, asthma, tuberculosis,thyroid anomalies
FAMILY HISTORY:
Not significant
PERSONAL HISTORY
Appetite: decreased
Diet : liquified food is given through ryles tube
Usually given foods are rice, dal with water.
Sleep: Adequate
Bowel and Bladder: Regular
Addictions: Used to drink alcohol and smoke occasionally
TREATMENT HISTORY:
Suction every 2 hourly.
Change in position every 2 hours.
Vitals monitoring every 4 hrs.
Tab RANITIDINE 150 mg PO/OD (morning before food)
T. LEVITARECITAM 500mg PO/OD (Night time)
T. SUPRA CAL [ CALCIUM CITRATE+VITAMIN K2-7+ CALCITRIOL ]PO/OD (after lunch)
GENERAL PHYSICAL EXAMINATION :
The patient is in a vegetative state, uncooperative, appears thin, weak, and malnourished
Pallor-absent
Icterus-absent
Cyanosis-absent
Clubbing-absent
Lymphadenopathy-absent
Pedal edema- absent
Koilonychia- absent
Burn scar present on left palmer surface due to electric scar.
VITALS:-
Temperature: 98°F
Pulse rate: 100 beats per minute
Respiratory rate:20 cycles per minute
Bp:105/80
Spo2: 98%
SYSTEMIC EXAMINATIONS
CENTRAL NERVOUS SYSTEM
GCS :- E4 V2 M4 At the time of examination
Higher mental functions
Patient is disoriented and is in vegetative state
Memory and speech could not be assessed.
Intellect cannot be assessed
Release reflexes
Grasp reflex:- couldn't be performed as patient kept his fists clenched
Glabellar reflex:- Absent
Pout reflex:- Absent
Palmo-mental reflex:- Couldnt be performed as patient kept his fists clenched
Cranial nerve examination
Pupillary reflex: Direct (present)
Indirect(present)
Corneal and conjunctival reflexes are present
Gag reflex is present
Motor System :-
Right Left
UL LL UL LL
Bulk wasted wasted wasted wasted
Tone hypertonia normal hypertonia normal
Power :- 3/5 3/5 3/5 3/5
Reflexes:-
Biceps, Triceps, and Supinator reflexes are absent
Knee reflex positive in both limbs
Ankle reflex positive in both limbs
plantar reflex positive in both limbs
sensory system: could not be elicited
myoclonic jerks are seen regularly
Gait: could not be elicited
CARDIOVASCULAR SYSTEM :
S1 and s2 are heard
No murmurs are heard
Trachea - central with tracheostomy tube
RESPIRATORY SYSTEM:
Bilateral basal crepitations are heard .
ABDOMINAL EXAMINATION:
Soft and non tender
liver and spleen not palpable
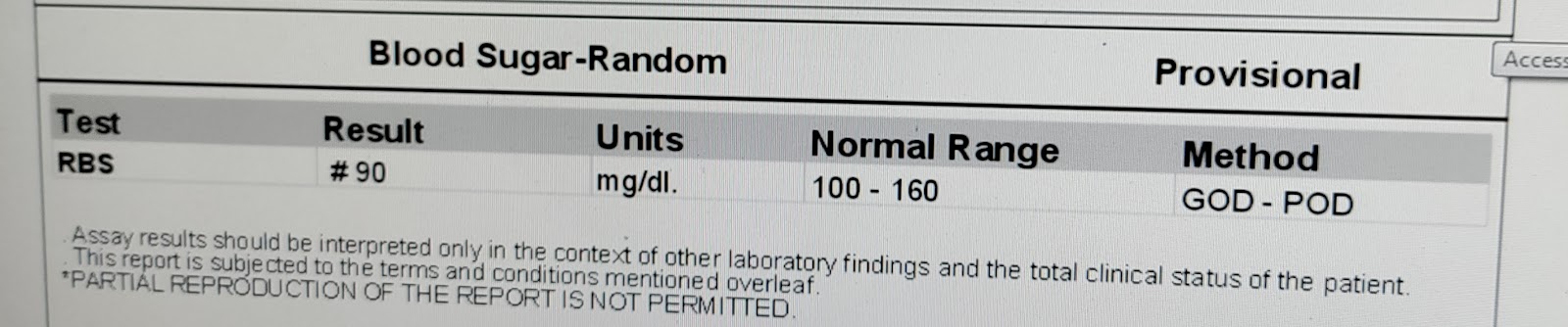
INVESTIGATIONS:
XRAY NECK
XRAY CHEST
PROVISIONAL DIAGNOSIS:
Hypoxic ischemic brain injury post cpr state
TREATMENT PLAN:
After a neurology consultation neurologist suggested family counseling and palliative therapy






Comments
Post a Comment